
Hip impingement, medically known as femoroacetabular impingement (FAI), is a condition where abnormal contact between the bones of the hip joint leads to pain and limited movement. Accurate diagnosis is crucial for effective treatment. This article explores the comprehensive approach used by healthcare professionals to diagnose hip impingement.
The diagnostic process begins with a thorough clinical history. Patients are asked about their symptoms, including the nature, location, and duration of pain. Common symptoms of hip impingement include:
Pain in the groin, thigh, or buttocks
Stiffness or limited range of motion in the hip joint
Pain exacerbated by activities such as squatting, twisting, or prolonged sitting
Understanding these symptoms helps healthcare providers determine the likelihood of hip impingement and guides further diagnostic steps.
A comprehensive physical examination is essential in diagnosing hip impingement. Healthcare providers perform specific maneuvers to assess hip function and identify signs indicative of impingement. Two commonly used tests include:
FADIR Test (Flexion, Adduction, Internal Rotation): The patient flexes the hip, brings it across the body (adduction), and internally rotates the leg. Pain during this maneuver suggests impingement.
FABER Test (Flexion, Abduction, External Rotation): The patient flexes the hip and knee, places the foot on the opposite knee, and allows the knee to drop toward the table. Pain or limited motion may indicate hip joint issues.
These physical tests help clinicians assess the hip’s range of motion and identify areas of discomfort, providing valuable information for diagnosis.
Imaging plays a pivotal role in confirming the diagnosis of hip impingement and assessing the extent of joint involvement. Common imaging modalities include:
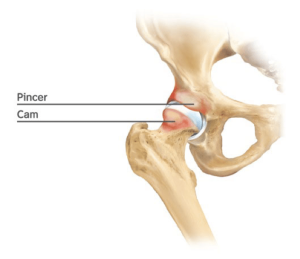
X-rays: Standard X-rays can reveal structural abnormalities such as cam or pincer deformities, which are characteristic of FAI.
MRI (Magnetic Resonance Imaging): MRI provides detailed images of soft tissues, including cartilage and labrum, helping to identify tears or damage.
MRI Arthrogram: Involves injecting a contrast dye into the hip joint before MRI imaging to enhance visualization of the labrum and cartilage.
These imaging techniques allow healthcare providers to visualize the hip’s internal structures, aiding in accurate diagnosis and treatment planning.
Several conditions can mimic the symptoms of hip impingement, making differential diagnosis crucial. Healthcare providers consider other potential causes of hip pain, such as:
Hip labral tears
Osteoarthritis of the hip joint
Tendinitis or bursitis
Muscle strains or ligament injuries
By ruling out these conditions through clinical evaluation and appropriate testing, providers can confirm hip impingement as the primary diagnosis.
Early diagnosis of hip impingement is vital to prevent long-term complications. If left untreated, FAI can lead to:
Progressive cartilage damage
Development of hip osteoarthritis
Chronic pain and disability
Timely intervention, including physical therapy, lifestyle modifications, or surgical options, can alleviate symptoms and improve joint function.
Diagnosing hip impingement involves a comprehensive approach, including detailed patient history, physical examination, and advanced imaging techniques. Accurate diagnosis is essential for developing an effective treatment plan to manage symptoms and prevent further joint damage. If you experience persistent hip pain or discomfort, consult a healthcare provider specializing in musculoskeletal disorders for a thorough evaluation.